We’ve all had occasional nasty stomach cramps. But if
abdominal pain is a daily occurrence for you, then youmay
have something called in ammatory bowel disease (IBD).
IBD is the name given to a set of conditions in which
parts of the gastrointestinal tract—usually the intestines—
become chronically inflamed, triggering abdominal
cramps, diarrhea and even bleeding in the intestines. e
two most common forms of IBD are Crohn’s disease and
ulcerative colitis.
Who is at risk?
IBD is most likely caused by a
malfunction in the immune system. Anyone can get IBD.
However, it occurs more o en among:
People who have a family member with IBD.
Ashkenazi Jews.
Caucasians.
People who live in northern climates, in cities or in
developed countries.
Smoking also increases the risk for Crohn’s disease.
e e ect of smoking on ulcerative colitis risk is unclear.
Symptoms
Most people who get IBD will begin to have
symptoms between the ages of 15 and 30. e severity of
symptoms can vary widely, and they can also come and go.
Typical signs and symptoms of IBD include: Severe or
chronic abdominal cramping or pain.
Diarrhea, which
may be bloody.
Blood in the stool.
Unexplained or
unintended weight loss. Loss of appetite. Pain in, or
bleeding from, the rectum. Joint pain. Fever. Fatigue.
Treatments
If you have IBD, treatment will depend on the
severity of your symptoms. Your doctor may recommend:
Medications.
IBD medications are used to reduce
in ammation, relieve symptoms and prevent are-ups.
Surgery.
About 65 to 75 percent of all people with
Crohn’s disease will have surgery for it at some point in
their lives. Procedures may relieve symptoms but are not
a cure. However, if you have ulcerative colitis, surgery to
remove your entire large intestine may eliminate your
disease. Between 25 and 40 percent of people who have
ulcerative colitis eventually need surgery.
See your doctor
By working closely with your doctor,
you can lead a full and healthy life.
Sources: American Academy of Family Physicians; American College of Gastroenterology;
Centers for Disease Control and Prevention; Of ce on Women’s Health
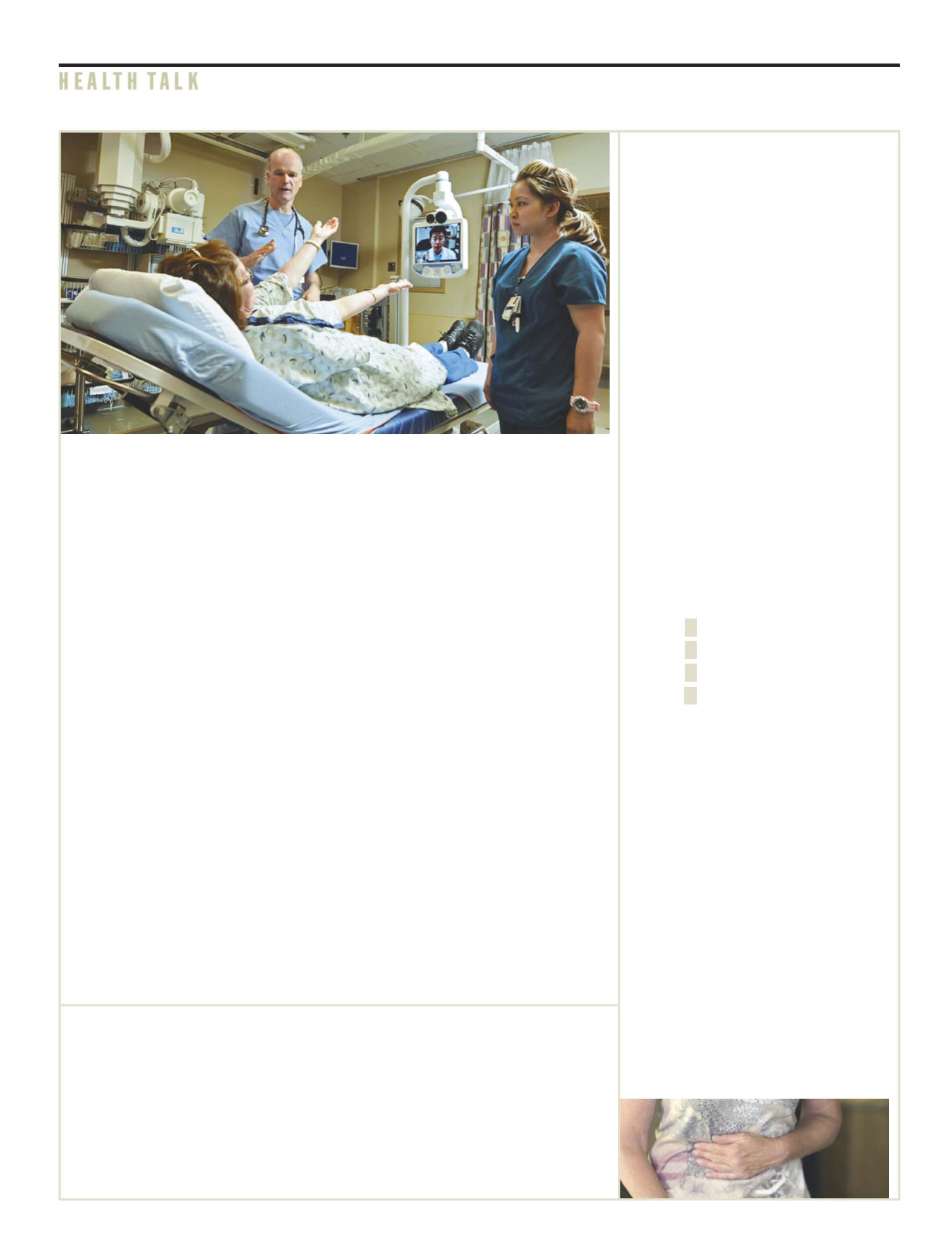
It’s amazing what digital technology
can do these days. In our everyday
lives, we can share our snapshots
immediately with friends or use a
webcam to both see and hear distant
relatives. In a similar way, technology
now in our emergency department is
helping us deliver timely stroke care.
Stroke is a leading cause of
disability and the third leading cause
of death. According to the Centers
for Disease Control and Prevention,
on average, one American dies from
stroke every four minutes. rough
the Tele-Stroke Program, Medina
Regional Hospital now has access to
Methodist Healthcare neurologists
who can remotely diagnose and treat
stroke patients when minutes count.
“This new network allows us
to offer acute stroke neurology
coverage 24 hours a day, 7 days a
week, 365 days a year,” says Janice
Simons, Medina Regional Hospital
CEO. “We are so grateful to Methodist
Healthcare for partnering with us for
this critical service. Our community
can be comforted in knowing that if
they experience stroke symptoms,
they can get effective, efficient
healthcare right here at their local
hospital within minutes of arrival.”
Tele-stroke uses a video conference
system and a web connection to link
our emergency department to stroke
specialists whenever their expertise
is needed. Without being physically
at the hospital, the specialists can
examine and speak with stroke
patients here and consult with our
physicians using equipment that
includes a webcam and video screen.
And the specialists are available 24
hours a day. is is essential because
time is crucial when someone is
having a stroke.
“ rough the Tele-Stroke Program,
physicians can dramatically increase
response time; transfers can be
minimized; and patients can o en
receive lifesaving care faster, o en
remaining at or near their home
hospital,” says Simons.
Most strokes happen when a
clot blocks blood ow to the brain,
robbing its cells of oxygen they need.
A clot-busting drug called tissue
plasminogen activator (tPA) can
restore blood ow and help prevent
disability in people who have these
strokes. To work best, it must be
given within three hours of the onset
of symptoms and only a er doctors
determine whether the patient is a
candidate for tPA. O en, making that
decision requires consultation from a
neurologist who specializes in strokes.
at’s where tele-stroke comes in.
When a person who may be having
a stroke arrives at the emergency
department, doctors can activate
the secure system to connect with
a remote neurologist if one is not
immediately available here. The
distant stroke team member can see
and hear the patient and emergency
department doctor, and vice versa.
The neurologist can do a stroke
exam, review brain scans, take a
patient history and work with the
emergency physician. e result is
a swi determination as to whether
tPA or other treatments are needed.
Be a partner—learn stroke signs
Learn stroke’s warning signs, and call
right away if you spot them in
yourself or someone else. ey come
on suddenly and include:
Numbness or weakness of the
face, arms or legs—especially on one
side of the body.
Confusion or trouble speaking or
understanding speech.
Trouble seeing.
Dizziness, loss of balance or
coordination, or trouble walking.
Severe headache with no obvious
cause.
Tele-stroke brings stroke specialists to you
Don’t ignore
stomach pains
ey may be in ammatory
bowel disease
Go to medinahospital.net to
learn about IBD expert Chris
Connaughton, MD, and other
visiting specialists.
Make your end-of-life wishes known
We can’t control how we enter this
world. But we can make some big
decisions about how we’d like to
leave it.
Deciding how you’d like to be
treated during this time can ensure
your life ends with dignity and
according to your values. You
can make your wishes concerning
your medical treatment known
before you actually need such care.
Advance directives are the legal
documents that allow you to do this
in accordance with Texas law.
Make an advance directive
You
can get a form from your healthcare
facility or download one online
in English or Spanish at
tha.org/
GeneralPublic/AdvanceDirectives/
index.asp
. Click on “What Are My
Options forAdvanceDirectives?”When
the form is complete, share copies
with your doctor and your family, and
take copies with you to the hospital.
Sources: American Academy of Family Physicians; National
Cancer Institute; National Hospice and Palliative Care
Organization; Texas Hospital Association
G
S P R I N G 2 0 1 4
M E D I N A H E A L T H N E W S
3
N E W S , V I E W S & T I P S
H E A L T H T A L K